A Closer Look at the Fentanyl Crisis
America’s overdose emergency has been shaped by many forces, but none has proved more lethal — or more elusive — than fentanyl, a synthetic opioid. Even as provisional data hint at a welcome decline in overall drug deaths, fentanyl still shadows nearly every state, community, and family affected by substance use disorders (SUDs).
Behind the headlines are interwoven public-health challenges: addiction, untreated mental illness, and the unique dangers facing people reentering their communities after incarceration. Understanding how these threads connect is the first step toward expanding residential, co-occurring treatment that saves lives.
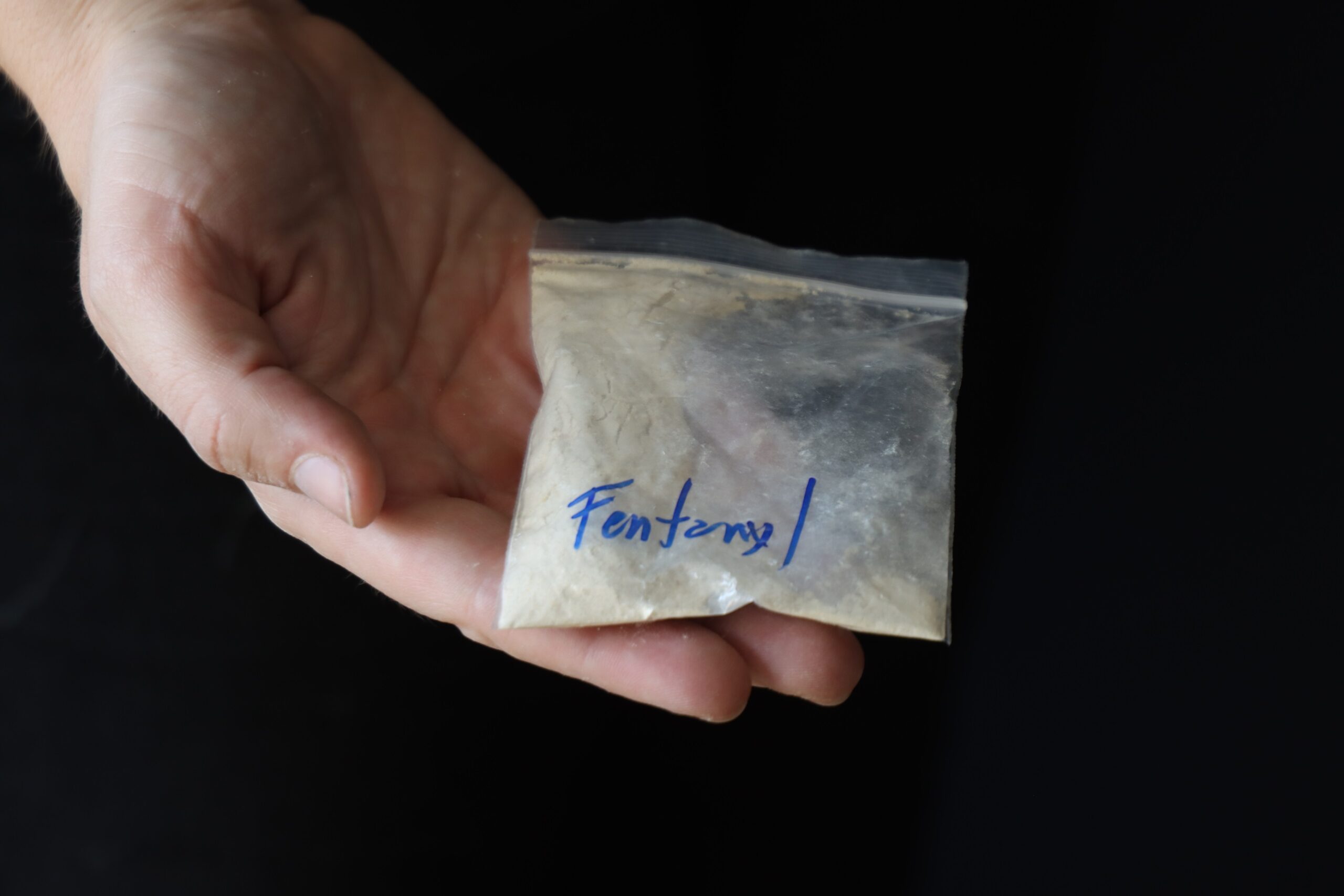
Fentanyl: Why a Milligram Matters
Fentanyl is 50 to 100 times stronger than morphine and cheap to manufacture, so traffickers increasingly press it into counterfeit pain pills or cut it into heroin, cocaine, and methamphetamine. The result is a drug supply littered with “one-pill-can-kill” land mines. In 2023, synthetic opioids — chiefly fentanyl — were implicated in more than 81,000 U.S. overdose deaths.
The Double Punch of Addiction and Mental Illness
Addiction seldom travels alone. Anxiety, depression, PTSD, and other conditions raise the risk of misusing opioids, while heavy opioid use can worsen or mask mental health symptoms. The relationship is fiercely bidirectional:
- Self-medication spiral: People often reach for dangerous substances in an attempt to blunt panic, numb intrusive thoughts, or chase sleep. In the short term, it may work, but withdrawal amplifies those very symptoms, pulling users deeper into dependence.
- Neurochemical hijacking: Repeated opioid exposure rewires dopamine and serotonin pathways, increasing vulnerability to mood disorders, impairing decision making, and heightening suicide risk.
- Stress and trauma overlap: Childhood adversity, combat experience, and community violence place the brain on constant alert, simultaneously elevating the odds of PTSD and opioid misuse.
Because the two disorders share symptoms such as restlessness, sleep disturbance, and hopelessness, one can hide behind the other, delaying diagnosis. Treating addiction without addressing anxiety, or vice versa, leaves neural circuitry primed for relapse and overdose. Co-occurring, residential treatment that tackles both conditions simultaneously is the optimal approach to tackle these problems.
Why Residential, Co-Occurring Treatment Works
Outpatient counseling helps many people, but fentanyl’s extreme potency raises the stakes. Residential programs that address mental health and addiction under one roof provide:
- A safe, sober setting that removes access to a toxic street supply.
- 24/7 medical oversight to manage withdrawal and monitor psychiatric symptoms.
- Integrated clinical teams trained in evidence-based therapies such as medication-assisted treatment (MAT), cognitive behavioral therapy, and trauma-informed care.
- Structured skill-building — from relapse-prevention planning to job preparation — that continues after discharge.
- Peer and family engagement, which research links to longer recovery.
These elements create a continuum that can outlast fentanyl’s lure and address the root causes of substance use.
The Crisis Behind Bars — and After Release
Incarcerated and formerly incarcerated individuals carry some of the heaviest burdens of untreated addiction and mental illness. Roughly 63 percent of individuals in jail and 58 percent in state prison meet the criteria for an SUD, while up to 44 percent suffer from a mental illness. Furthermore, overdose risk skyrockets upon release; studies show the odds of a fatal opioid overdose are more than ten times higher during the first two weeks after leaving custody than for the general population. Fentanyl intensifies that danger: a single relapse dose can prove deadly to someone whose tolerance dropped while incarcerated.
Formerly incarcerated individuals also face systemic barriers — unstable housing, limited employment options, and loss of social support — that amplify stress and erode mental health. Without coordinated discharge planning and immediate pathways to comprehensive treatment, many fall through the cracks, and prisons become a revolving door.
Closing the Treatment Gap
Expanding residential, co-occurring programs is crucial, but scale alone won’t solve the fentanyl crisis. Policymakers, insurers, and communities must also:
- Fund effective treatment inside correctional facilities and ensure continuity of care post-release.
- Support housing-first models that give people a stable address while they engage in treatment.
- Invest in culturally responsive care, recognizing that overdose trends disproportionately affect Black, Indigenous, and rural populations.
- Reduce stigma by framing SUD and mental illness as treatable health conditions, not moral failings.
Find Help at Pioneer Human Services
For more than 60 years, Pioneer Human Services has stood at the intersection of recovery and reentry. Our residential programs offer integrated treatment for substance use and mental health disorders, and robust reentry support, helping clients build the skills and confidence to thrive in their community. If you or a loved one is battling fentanyl or other substances, explore our treatment services and start your journey to healing with Pioneer Human Services.
Pioneer Human Services empowers justice-involved individuals to overcome adversity and reach their full potential. With over 35 programs across the state of Washington, we’re working to eradicate mass incarceration through innovative programs and social entrepreneurship. Support our work today, and help us provide counseling, career services, housing, and — most importantly — hope.
